Maternal mortality remains a pressing concern, especially in high-income countries like the United States, where alarming statistics reveal that pregnancy-related deaths continue to rise. This increase highlights serious issues within maternal health, including inadequate prenatal and postpartum care that could significantly reduce maternal fatalities. Recent studies show that preventable causes account for more than 80% of these tragic outcomes, underscoring the urgent need for comprehensive reforms in our healthcare system. Disparities based on race, state, and socioeconomic status further complicate the landscape, making it imperative to address these multifaceted challenges head-on. By prioritizing effective strategies for reducing maternal mortality, we can work towards a health system that ensures safer pregnancies for all women, no matter their background.
The phenomenon of maternal mortality, also known as pregnancy-related death, reflects a critical aspect of public health that requires urgent attention. Defined broadly as the deaths caused by complications during pregnancy or within the first year following childbirth, this issue underscores the need for enhanced maternal healthcare services. In many regions, maternal health systems are under severe strain, leading to significant rates of preventable deaths. Factors such as late maternal deaths, often overlooked, play a pivotal role in understanding the full scope of maternal health challenges. As we delve deeper into this topic, the urgent call for systematic improvements and equitable care becomes increasingly clear.
Understanding Maternal Mortality Rates in the U.S.
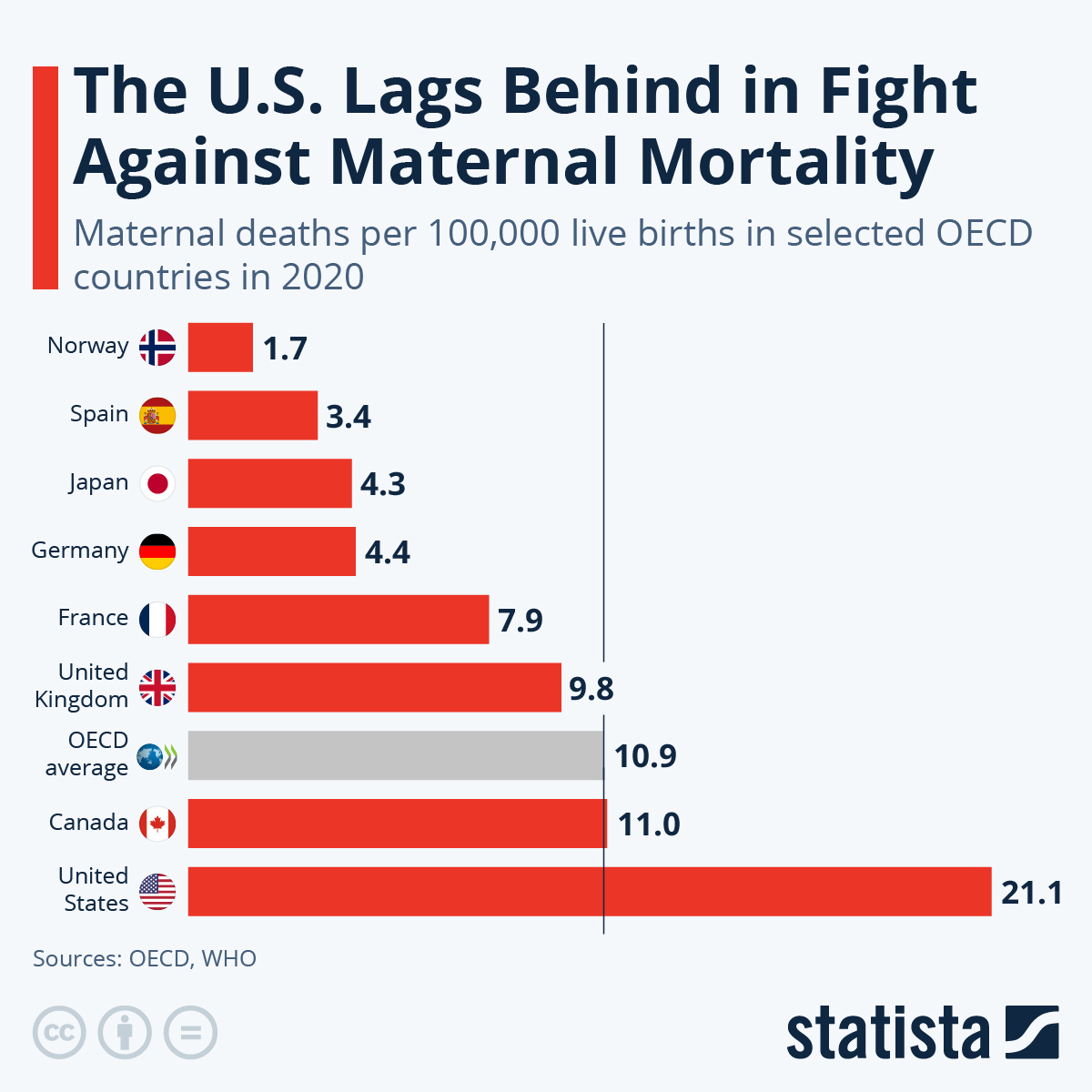
Maternal mortality refers to deaths that occur due to complications from pregnancy or childbirth, and the United States has some of the highest rates among high-income countries. Recent data shows that in 2022 alone, the U.S. recorded 32.6 maternal deaths per 100,000 live births, starkly higher than the rates in other developed nations. This troubling statistic emphasizes a failure of the healthcare system that requires immediate, multifaceted intervention. The rise in maternal mortality rates, particularly during the COVID-19 pandemic, sheds light on systemic flaws in prenatal care, which need to be addressed to prevent further loss of life.
The increase in maternal mortality is disproportionately impacting women of color, particularly American Indian, Alaska Native, and Black women, who face mortality rates significantly higher than their white counterparts. This disparity can largely be attributed to a combination of inequitable access to healthcare, socioeconomic factors, and systemic biases within medical practices. Reducing maternal mortality will require targeted policies aimed at improving maternal health outcomes across all racial and ethnic groups and ensuring that everyone has equal access to quality care.
The Impact of Chronic Conditions on Maternal Health
Research indicates that chronic medical conditions such as hypertension and diabetes are increasingly affecting younger women, contributing significantly to the rise in pregnancy-related deaths. Unlike previous generations, women aged 25 to 39 are now more likely to suffer from cardiovascular diseases during pregnancy. This demographic shift highlights the importance of integrating comprehensive healthcare solutions that address chronic conditions prior to and during pregnancy. Better screening and management practices could be effective strategies in reducing the incidence of pregnancy-related complications.
Healthcare providers must prioritize early intervention strategies targeting chronic diseases among women of reproductive age. This includes enhancing access to preventative care and education about managing conditions like weight, hypertension, and diabetes before conception. By directly addressing these risk factors, it may be possible to lower maternal morbidity and mortality rates, ensuring that pregnancies can proceed without the side effects of unmanaged health conditions.
The Role of Postpartum Care in Maternal Health
Postpartum care, the healthcare women receive after giving birth, is critical in addressing maternal health and reducing mortality rates. Current research suggests that a significant portion of maternal deaths occur after the initial 42 days postpartum, indicating that many health systems overlook the long-term recovery of mothers. By extending the focus of postpartum care to at least one year after childbirth, healthcare providers can better support women in their recovery phase and reduce late maternal deaths.
Integrating comprehensive postpartum care involves not just routine check-ups but also mental health services, education on physical recovery, and ongoing monitoring of chronic conditions. Attention must shift to developing tailored care plans that consider both the physical and emotional well-being of mothers, emphasizing the importance of a continuum of care that persists beyond the conventional six-week follow-up. This approach could significantly impact women’s health outcomes and assist in reducing overall maternal mortality rates.
Addressing Racial Disparities in Maternal Mortality
Racial disparities in maternal mortality remain a pressing issue, with women of color experiencing significantly higher rates of pregnancy-related deaths compared to white women. The study shows that American Indian and Alaska Native women are the most affected, followed by Black women. Addressing these disparities requires a concerted effort towards equitable healthcare policies and practices, ensuring that all women, regardless of their race or socioeconomic status, receive high-quality maternal care.
Efforts to mitigate these disparities should include increasing representation in healthcare, culturally competent care, and community-based programs that directly address the unique needs of diverse populations. By focusing on equity in maternal health, we can create a more inclusive system that not only safeguards the health of mothers during pregnancy but also supports them effectively in their postpartum period.
The Importance of Data in Improving Maternal Health Outcomes
Collecting accurate data on maternal mortality is essential for understanding the scope of the issue and for developing targeted interventions. The recent inclusion of a pregnancy checkbox on death certificates has enhanced the ability to track maternal deaths more systematically. However, further investment in public health infrastructure is critical to ensure comprehensive understanding and addressing of maternal health challenges.
Inconsistent data collection has previously hindered efforts to fully realize the impact of maternal mortality across states and demographics. As healthcare reporting continues to improve, researchers and policymakers must use this data to inform public health strategies that aim not just to reduce maternal mortality but to foster overall better maternal health outcomes. Continuous monitoring and targeted policy changes based on data findings are key to driving down pregnancy-related deaths.
Investing in Preventative Healthcare to Reduce Pregnancy-Related Deaths
Preventative healthcare is paramount in addressing the alarming rates of pregnancy-related deaths in the U.S. Systematic improvements in prenatal care, maternal health education, and proactive management of pre-existing medical conditions are essential steps towards equipping mothers with the necessary tools for a healthy pregnancy. Women need access to resources that promote healthy lifestyles before and during their pregnancy to minimize the chances of complications.
In addition, funding programs aimed at educating women about the importance of regular health check-ups and lifestyle management could significantly enhance maternal health. By bridging the gap between awareness and practice, it’s possible to reduce the burden of chronic health conditions that often lead to pregnancy-related complications and ultimately fatalities.
Innovative Solutions for Enhanced Maternal Care
The rising rates of maternal mortality highlight the urgent need for innovative solutions within healthcare systems. These solutions could include telemedicine, which expands access to maternal healthcare for women in rural or underserved areas, allowing them to receive timely consultations and support. Additionally, integrating technology in prenatal monitoring can help detect red flags that might indicate complications, enabling healthcare providers to intervene early.
Moreover, the development of community-based health programs that focus on holistic maternal care could greatly enhance support systems for pregnant women. Such programs can connect mothers with essential resources, including nutrition advice, mental health services, and comprehensive health screenings, which are critical for long-term maternal health. By harnessing innovation in healthcare delivery, we can create a more responsive system that significantly improves maternal health outcomes.
Policy Changes Needed to Support Maternal Health
To effectively tackle the issue of maternal mortality, policymakers must implement significant changes within the healthcare system. This includes allocating resources towards equitable maternal health programs, enhancing training for healthcare providers on cultural competency, and ensuring access to care regardless of socioeconomic status. Additionally, comprehensive health insurance coverage that encompasses both prenatal and postpartum care is essential for encouraging consistent healthcare access.
Furthermore, addressing social determinants of health, such as housing, education, and access to transportation, is crucial in reducing maternal health disparities. By creating policies that address these broader issues, the healthcare system can start to see improvements in maternal health outcomes and work towards reducing the high rates of preventable pregnancy-related deaths.
Community Engagement in Maternal Health Improvement
Community engagement is vital for enhancing maternal health outcomes and efforts to reduce maternal mortality rates. Programs designed to involve local communities in maternal healthcare initiatives can help address unique health challenges specific to their populations. Community health workers can play a fundamental role in bridging gaps between healthcare services and mothers, offering support and education about available resources.
By establishing trust and open communication between healthcare providers and communities, we can ensure that maternal care is culturally relevant and accessible. Outreach programs that prioritize community involvement can facilitate better health outcomes and foster environments that empower women to advocate for their own health needs throughout their pregnancy and postpartum journey.
Frequently Asked Questions
What are the main causes of maternal mortality in the U.S.?
The leading causes of maternal mortality in the U.S. include cardiovascular disease, hemorrhage, and infections. Over the years, the transition from hemorrhage to cardiovascular issues has made heart-related conditions a significant contributor, particularly among women between the ages of 25 to 39. Addressing chronic conditions like hypertension is crucial to reducing maternal mortality rates.
How does the U.S. maternal mortality rate compare to other high-income countries?
The U.S. has the highest maternal mortality rate among high-income countries, with pregnancy-related deaths consistently rising. Factors contributing to this include healthcare inequities, access to prenatal care, and systemic biases affecting racial and ethnic groups.
What role does postpartum care play in reducing maternal mortality?
Postpartum care is vital in reducing maternal mortality, as it addresses health issues that may arise during the extended postpartum period, which is recognized as encompassing up to one year after birth. Improved postpartum care can help identify and manage complications that contribute to late maternal deaths.
What are the disparities in maternal mortality rates among different racial groups in the U.S.?
Significant disparities in maternal mortality rates exist among racial groups in the U.S. For instance, American Indian and Alaska Native women experience the highest rates at 106.3 deaths per 100,000 live births, compared to 27.6 for white women and 76.9 for non-Hispanic Black women. These disparities underscore the need for targeted interventions in maternal health.
How can investing in maternal health care help reduce pregnancy-related deaths?
Investing in maternal health care can enhance the quality of care during pregnancy and the postpartum period, ultimately reducing pregnancy-related deaths. Addressing healthcare system design and policy differences among states is essential to ensure equitable access to comprehensive maternal health services.
Why is late maternal death an important factor in maternal mortality statistics?
Late maternal deaths, occurring from 42 days to one year postpartum, are significant as they represent nearly a third of total maternal deaths in the U.S. Recognizing this period is important for improving care and support during recovery, which can help prevent these deaths and provide a more accurate picture of maternal health outcomes.
What changes are necessary to address the rising maternal mortality rates in the U.S.?
To address rising maternal mortality rates, it is crucial to enhance public health infrastructure, invest in innovative health solutions, and enforce policies that reduce healthcare inequities. Moreover, understanding the underlying factors that contribute to state-level disparities can inform targeted actions to improve maternal health outcomes nationwide.
What is the impact of chronic health conditions on maternal mortality?
Chronic health conditions, such as hypertension and diabetes, significantly impact maternal mortality rates by increasing the risk of complications during pregnancy. The increasing incidence of these conditions in younger populations highlights the need for early intervention and management to improve maternal health.
How does maternal health care access vary between states?
Maternal health care access varies significantly between states, with some states showing much higher maternal mortality rates due to differing policies, resource distribution, and healthcare quality. Reducing these variations is essential for improving overall maternal health outcomes across the U.S.
What role does education and public awareness play in reducing maternal mortality?
Education and public awareness are critical in reducing maternal mortality by informing women about the importance of prenatal and postpartum care. Increased awareness can empower women to seek care and manage their health, which is essential in preventing pregnancy-related complications.
| Key Points | |
|---|---|
| Rising Maternal Mortality | The U.S. has the highest maternal mortality rate among high-income countries, continuing to rise, especially during 2021, coinciding with the COVID-19 pandemic. |
| Preventable Deaths | Over 80% of pregnancy-related deaths are preventable according to research from NIH. |
| Racial Disparities | American Indian women have the highest mortality rates, with significant disparities across racial groups. |
| Health System Issues | Inequitable healthcare access and systemic bias contribute to high maternal mortality rates. |
| Chronic Conditions | Increased rates of cardiovascular diseases and chronic conditions are recorded in younger populations. |
| Late Maternal Deaths | Almost a third of maternal deaths occur between 42 days to 1 year postpartum. |
| Policy Recommendations | Investment in public health and innovative healthcare solutions is essential to reduce maternal mortality. |
Summary
Maternal mortality remains a critical issue, with the U.S. exhibiting alarmingly high rates compared to other high-income nations. Addressing maternal mortality requires a multifaceted approach, including better healthcare access, addressing racial disparities, and enhancing care throughout the postpartum period. By prioritizing these areas and investing in public health infrastructure, the U.S. can make significant strides toward reducing preventable deaths related to pregnancy.