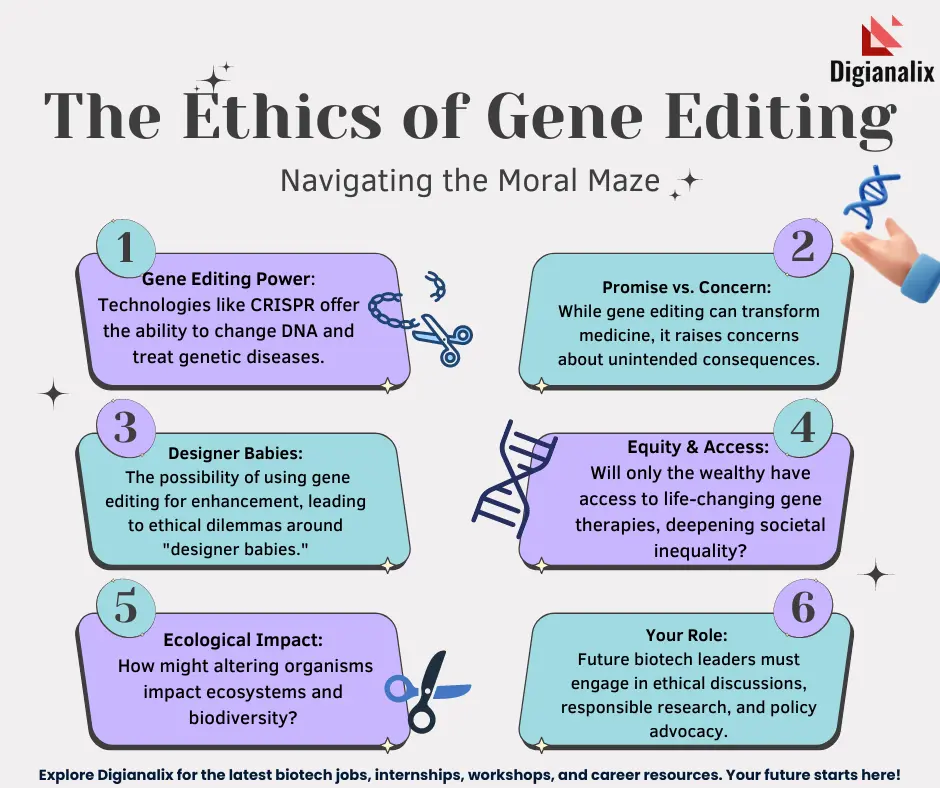
Gene editing ethics raises profound questions as revolutionary technologies like CRISPR continue to reshape our approach to health and disease. At the forefront of this bioethics discussion is the potential to eradicate conditions such as sickle cell disease, sparking debates about the moral implications of genetic manipulation. As we stand on the brink of such medical advancements, we must consider issues of health equity and access to these technologies. With CRISPR’s ability to modify germline cells, the possibility of heritable changes complicates our understanding of what it means to be human. The intersection of innovation and ethics demands a careful examination of the societal impacts of gene editing, ensuring that we do not sacrifice our ethical responsibilities in pursuit of medical breakthroughs.
The ethical landscape surrounding gene modification and editing is as complex as the genetic structures it aims to alter. Modern advancements in genetic technology now enable scientists to address various health challenges, from hereditary diseases to genetic disorders. This intersection of science and morality invites an urgent discussion about how we manage the implications of altering genetic material. Concepts like health justice and equitable access become increasingly important as we navigate the potential benefits and risks involved. Engaging in this conversation helps us to understand our responsibilities towards future generations and reinforces the need for ethical guidelines in the field of genetic research.
The Promise of CRISPR Technology in Treating Sickle Cell Disease
CRISPR technology represents a groundbreaking leap in the field of genetic manipulation, particularly in the treatment of genetic disorders like sickle cell disease. This revolutionary gene editing tool allows scientists to precisely target and edit the genes responsible for diseases, potentially offering a cure for individuals suffering from conditions that have long been deemed untreatable. By using CRISPR to modify the genes in somatic cells, medical professionals can alleviate the symptoms of sickle cell disease, thus drastically improving patients’ quality of life. As the technology advances, the potential to edit the germline genes raises even more intriguing possibilities, allowing for the eradication of the disease at its source.
However, the implementation of such technology is fraught with ethical considerations. While the prospect of curing a painful condition like sickle cell disease is enticing, it raises significant questions about the societal implications of gene editing. Who gets access to these treatments, and at what cost? Many argue that without careful oversight and consideration for health equity, the benefits of CRISPR technology may not extend to all, particularly marginalized communities. As healthcare systems grapple with these disparities, the promise of CRISPR must be balanced against the realities of access and cost, amplifying the bioethics discussion surrounding genetic interventions.
Navigating Gene Editing Ethics: A Bioethics Discussion
At the forefront of the conversation surrounding gene editing is the ethical dilemma of whether humanity should alter what is considered ‘normal’ in the context of human variation. The discussions led by bioethics experts like Rebecca Weintraub Brendel raise critical questions about our moral obligation to utilize CRISPR technology to treat genetic disorders, particularly in cases of non-life-threatening conditions. As seen in the cases discussed, such as genetic modifications made for children of deaf parents, decisions about these alterations can provoke deep ethical debates regarding autonomy, parental rights, and the definition of disability. These discussions emphasize the need for comprehensive ethical guidelines to navigate this rapidly advancing field.
Moreover, the ethical implications extend beyond individual choices to include wider societal concerns about the ramifications of genetic manipulation. The potential for CRISPR technology to create a societal divide—where the wealthy can afford enhancements while the poorer populations remain untreated—highlights the critical importance of integrating health justice into the conversation. As institutions begin to adopt gene editing, it is vital that policies address the potential disparities created by this technology, ensuring that innovations do not exacerbate existing inequalities in health care and access. The discussions emphasize the urgency of aligning scientific advancement with equitable access and ethical considerations.
Health Equity Challenges in Gene Editing
The introduction of CRISPR-based therapies into clinical practice has raised significant questions regarding health equity, particularly relating to the costs associated with these innovative treatments. For individuals suffering from sickle cell disease, the cure using CRISPR comes with a staggering price tag of approximately $2.2 million; a cost that seems prohibitive for many. As Neal Baer pointed out, the limited number of patients who could afford such treatments only serves to highlight the discrepancies in access to advanced medical technologies. This raises critical questions about how health systems can address these disparities, ensuring that breakthroughs in medical science benefit all, not just the privileged.
In addition to high costs, the conversation extends to the ethical implications of who gets prioritized in terms of treatment. As genetic manipulation capabilities expand, we must ensure that solutions are not only accessible to affluent populations but are also equitably distributed across all demographics. This involves a careful examination of policy-making processes to integrate considerations of race, socioeconomic status, and geographical disparities into the rollout of gene-editing therapies. Achieving health equity in this age of transformation requires a commitment from healthcare providers, policymakers, and society to address the barriers that disenfranchised populations face and to dismantle existing inequities.
Unintended Consequences of Gene Editing
The advancement of CRISPR technology raises significant concerns about the unintended consequences that may arise from gene editing. While the potential benefits are immense, the genetic complexities involved in manipulating genes can lead to unforeseen effects on human health. For example, when editing the LDL cholesterol gene to potentially reduce the risk of heart disease, there may be hidden repercussions that complicate metabolic processes in the body. As Baer pointed out, genes are intricately linked to various biological functions developed over billions of years, and altering one can create a ripple effect that goes beyond our immediate understanding.
Moreover, the excitement surrounding the potential of gene editing often overshadows the need for comprehensive research and monitoring to anticipate and mitigate these risks. As CRISPR technology becomes more accessible, the emphasis on safety and ethical oversight must be paramount. Without adequate regulation, the possibility of misuse or reckless experimentation could lead to detrimental effects on individuals and future generations. Understanding these potential unintended consequences is crucial as we advance in the realm of genetic manipulation, and it necessitates a dialogue that includes scientists, ethicists, and the public to ensure responsible and safe utilization of this powerful technology.
Oversight and Regulation in Gene Editing
The lack of robust oversight in the field of gene editing raises important concerns regarding the safety and ethical application of CRISPR technology. While many countries have established regulations on genetic engineering, there remains a disparity in enforcement and monitoring, particularly in regions where oversight is less stringent. The examples of potential misuse in countries without adequate regulations, such as China and Russia, highlight the risks that could arise from unregulated experimentation. Genetic enhancements conducted without proper ethical frameworks can lead to outcomes that not only jeopardize individual health but also pose broader societal implications.
Moreover, the debate surrounding oversight extends to questions about the nature of genetic interventions—should germline modifications be allowed? The crux of this issue lies in the morality of altering human genetics that can be passed down through generations. It invites discussions on the limits of scientific intervention and the responsibilities of researchers, governments, and society at large. Developing comprehensive regulatory frameworks is essential to ensure that gene editing is conducted responsibly and ethically, and that the advancements are harnessed for the greater good while minimizing risks to individual rights and societal integrity.
Innovations in Gene Therapy and Their Impact
Innovations in gene therapy using CRISPR technology have the potential to revolutionize treatment for a myriad of genetic disorders beyond just sickle cell disease. As researchers continue to uncover the intricacies of genetic pathways and their implications for various diseases, the hope is to develop targeted therapies that can effectively mitigate or cure conditions that were previously untreatable. These advancements underscore the importance of ongoing research and investment in gene therapy, as they could lead to breakthroughs for conditions like cystic fibrosis, muscular dystrophy, and certain types of cancer.
However, as these innovations come to fruition, it is crucial that the focus remains on responsible application and accessibility. As highlighted in discussions surrounding health equity, emerging therapies must not only be effective but also affordable and accessible to all populations. Tailoring approaches that consider the socioeconomic factors affecting treatment adoption will be fundamental in ensuring that these innovations fulfill their potential without exacerbating health disparities. By maintaining a balanced approach to gene therapy, we can aspire to create a future where advances in medicine benefit everyone, fostering health equity in the process.
The Intersection of Medical Innovation and Ethical Responsibility
The intersection of medical innovation and ethical responsibility is a crucial area of discussion as CRISPR and other gene-editing technologies advance. The ability to potentially eradicate diseases poses not only scientific and medical challenges but also ethical dilemmas that cannot be ignored. This interplay between the promise of scientific capability and the moral implications it carries underscores the importance of rigorous ethical scrutiny. As we navigate these waters, it becomes vital to engage a variety of stakeholders in the dialogue, including ethicists, healthcare providers, patients, and policymakers, to ensure a well-rounded perspective on the implications of these technologies.
Moreover, ethical calls to action demand that we prioritize deliberation over rapid implementation. While the excitement surrounding gene editing can spur remarkable advancements, it also creates a potential for hasty decisions that may not consider the long-term consequences. By fostering an environment that encourages comprehensive discussion about the responsibilities that come with such powerful technologies, we create pathways for informed decision-making that aligns scientific exploration with societal values. This concerted effort will help ensure that innovations in gene editing are not only pursued for their benefits but are also tempered with an understanding of their broader ethical context.
Parental Rights and Genetic Modifications
The question of parental rights in the context of genetic modifications is a delicate and multifaceted issue that evokes strong opinions and ethical dilemmas. With the advent of CRISPR technology, parents today may be faced with decisions about whether to edit genes in their unborn children based on potential inheritable conditions. Some advocate for the right of parents to make such decisions, arguing that it reflects a desire to spare their children from suffering. Yet, this raises profound questions about the extent of parental authority over a child’s genetic make-up and the societal implications of choosing certain traits over others.
Further complicating this discussion is the concept of what constitutes ‘normal’ or ‘desirable’ traits. Differentiating between curing diseases and enhancing desirable characteristics blurs the lines of ethical decision-making. As seen in the case of parents wanting to modify their children’s abilities or physical characteristics, it is essential to question who defines these traits and based on what criteria. This underscores a larger need for a framework to guide such decisions, ensuring that parental freedoms do not infringe upon the autonomy of the child or contribute to societal divides based on genetic enhancements. By engaging with the bioethical implications of these choices, society can move toward a more thoughtful approach to genetic modifications.
Global Perspectives on Gene Editing
As CRISPR technology advances, it is not just a national conversation but a global one, with countries around the world exploring the implications of gene editing. Variations in regulatory frameworks and cultural attitudes towards genetic manipulation raise critical questions about the direction of bioethics and international collaboration in the field. In some regions, stringent regulations may stifle innovation, while in others, lack of oversight can lead to unethical practices. This disparity calls for a coordinated international dialogue to establish universal ethical standards and guidelines governing the use of gene editing across borders.
Additionally, global health equity must be a key consideration in discussions surrounding gene editing. For countries with fewer resources, access to cutting-edge treatments and technologies can often be out of reach. As gene editing technologies become more prominent, efforts must be made to ensure that innovations are accessible to populations worldwide, including those in resource-limited settings. Encouraging collaborations between nations and organizations can foster shared knowledge and equitable access to treatment, allowing for a more inclusive approach to genetic healthcare that recognizes and addresses international disparities.
Frequently Asked Questions
What are the ethical considerations surrounding CRISPR technology in gene editing?
The ethical considerations surrounding CRISPR technology include questions of consent, safety, and sociocultural implications. As gene editing can alter genetic material permanently, concerns arise about unintended consequences, especially in germline editing where changes are passed on to future generations. There’s a significant bioethics discussion on whether we should edit genes for traits or conditions that are considered ‘compatible with life’, challenging notions of normalcy and human variation.
How does gene editing impact health equity, especially concerning sickle cell disease treatment?
Gene editing, particularly in treating diseases like sickle cell disease with CRISPR technology, raises critical health equity issues. The high cost of genetic manipulation—around $2.2 million for treatment—makes access limited primarily to affluent patients, thus exacerbating disparities. It prompts questions about who can afford such treatments and how solutions can be made accessible globally, ensuring that innovations do not solely benefit the wealthy.
Should parents have the right to use genetic manipulation to select traits for their children?
The question of whether parents should use genetic manipulation to select traits for their children opens a complex bioethics discussion. Critics argue that it may lead to a new form of eugenics, where societal pressures dictate desirable traits. Proponents, however, might argue for parental autonomy in making decisions for their children’s health and well-being. This dilemma underscores the balance between ethical responsibility and personal choice within gene editing practices.
What are potential risks associated with gene editing technologies like CRISPR?
Potential risks of gene editing technologies, including CRISPR, involve unintended genetic consequences and long-term health effects that we do not fully understand. Editing genes, especially those that have evolved over billions of years, can lead to unforeseen interactions within the genome, complicating outcomes. Furthermore, lack of regulatory oversight in some countries raises alarms about misuse or harmful applications of these powerful technologies.
How can the medical community ensure ethical practices in gene editing?
The medical community can ensure ethical practices in gene editing by establishing clear guidelines and ethical frameworks that prioritize patient welfare, informed consent, and equitable access. Ongoing bioethics discussions, inclusive stakeholder engagement, and international cooperation are essential to address the diverse implications of genetic manipulation, ensuring that innovations contribute positively to public health and do not perpetuate societal inequalities.
| Key Point | Details |
|---|---|
| Gene Editing Capabilities | CRISPR allows editing of somatic and germline genes, enabling cures for genetic diseases like sickle cell anemia. |
| Ethical Questions | Debates on the moral implications of editing genes for conditions like Down syndrome and the roles of parents in such decisions. |
| Costs and Equity | The high cost of gene treatments raises issues of fairness and health equity, especially for global populations. |
| Unintended Consequences | Gene editing can lead to unpredictable effects because genes interact in complex ways. |
| Regulatory Oversight | Concerns exist about the monitoring of gene editing practices in countries with lax regulations. |
Summary
Gene editing ethics presents complex moral dilemmas as the potential to cure genetic conditions like sickle cell disease clashes with questions of responsibility, oversight, and fairness. As scientists harness CRISPR technology to alter the very fabric of our biology, society must navigate these turbulent waters carefully, considering the implications not just for individuals, but for the collective human experience. This conversation must prioritize ethical considerations to ensure that innovations in gene editing serve to enhance health equity and justice rather than exacerbate existing disparities.