TIM-3 therapy for Alzheimer’s is an exciting advancement in the quest for effective Alzheimer’s treatment, leveraging the body’s immune system to combat this devastating disease. Recent research has revealed that manipulating the immune checkpoint molecule TIM-3 can free microglia, the brain’s resident immune cells, allowing them to attack the harmful plaques associated with Alzheimer’s. This innovative immune therapy for Alzheimer’s demonstrates the potential for a paradigm shift in how we approach the treatment of neurodegenerative diseases. Unlike traditional methods that focus solely on plaque removal, TIM-3 therapy combines the principles of cancer treatment for dementia with immunology, targeting the very processes that hinder cognitive function. As studies progress, the implications of TIM-3 in reshaping Alzheimer’s treatment strategies appear increasingly promising.
The TIM-3 molecule, an immune checkpoint involved in regulating microglial activity, presents a novel target for therapeutic intervention against Alzheimer’s disease. By inhibiting TIM-3, researchers aim to enhance the functionality of microglia, which play a crucial role in clearing amyloid-beta plaques from the brain. This approach represents a shift towards immune-based strategies, blending insights from cancer therapies with the challenges of dementia treatment. As scientists explore the genetic aspects of TIM-3 and its impact on Alzheimer’s patients, new horizons for improving cognitive health and memory restoration are emerging. The integration of immune modulation into Alzheimer’s research could revolutionize our understanding and management of this complex disorder.
The Role of Checkpoint Molecules in Alzheimer’s Disease
Checkpoint molecules, such as TIM-3, play a significant role in regulating the immune response within the brain. In healthy individuals, these molecules act as a form of brake to prevent the immune system from becoming overly active, which can lead to damage to the body’s own tissues. In the case of Alzheimer’s disease, however, an overexpression of TIM-3 on microglia, the primary immune cells of the brain, prevents these cells from clearing amyloid plaques. As a result, the accumulation of these plaques contributes to neurodegeneration and cognitive decline, characterizing the progression of Alzheimer’s. Understanding the balance that checkpoint molecules maintain is crucial in developing effective immunotherapies for Alzheimer’s treatment.
With the recognition that TIM-3 suppresses microglial activity, research is now focused on how inhibiting this checkpoint molecule can enhance the immune response in Alzheimer’s disease. By reducing the TIM-3 expression on microglia, these immune cells can potentially regain their ability to engulf and clear toxic plaques. The relationship between checkpoint molecules and Alzheimer’s emphasizes the need for targeted immune therapy strategies that can modify the immune landscape in the brain. This research not only opens pathways for new Alzheimer’s treatments but also sheds light on the disease’s complex interactions within the immune system.
Microglia and Their Functions in Alzheimer’s Pathology
Microglia are crucial for maintaining brain health, as they are responsible for clearing debris, regulating inflammation, and pruning synapses during development. In Alzheimer’s disease, however, their role becomes detrimental. The overexpression of checkpoint molecules like TIM-3 marks a shift in microglia from being effective cleanup agents to more passive participants in neurodegenerative processes. When microglial cells remain inactive due to TIM-3’s inhibitory effects, they fail to eliminate amyloid beta plaques, which leads to synaptic loss and cognitive impairment. Understanding the dysregulation of microglia in Alzheimer’s provides a critical insight into potential therapeutic approaches.
In studies involving mouse models of Alzheimer’s, researchers have demonstrated that deleting the TIM-3 gene from microglia can actively promote the clearance of amyloid plaques and restore cognitive functions. This suggests that therapies aimed at modifying microglial behavior could pave the way for innovative treatments. The focus on microglia and their interaction with checkpoint molecules like TIM-3 underscores the potential of immune therapies in Alzheimer’s treatment, which could transform how this debilitating condition is approached in clinical settings.
Innovative TIM-3 Therapy for Alzheimer’s
The concept of using TIM-3 therapy for Alzheimer’s disease represents a groundbreaking approach in neurology. This therapy could involve the use of anti-TIM-3 antibodies or small molecules designed to block TIM-3’s inhibitory effects, thereby enabling microglia to function effectively in clearing amyloid plaques from the brain. With promising results observed in mouse models, this strategy not only targets the cognitive decline seen in Alzheimer’s but also aims to prevent further plaque accumulation. Innovations in TIM-3 therapy could set a precedent for leveraging the body’s immune system in combating neurodegenerative diseases.
What distinguishes TIM-3 therapy is its dual purpose: it seeks to enhance the brain’s natural ability to clear toxic substances while also potentially improving cognitive functions. Given that a substantial percentage of Alzheimer’s cases are late-onset, targeting the mechanisms influenced by molecules like TIM-3 could be particularly impactful for an aging population facing dementia. As research progresses, TIM-3 therapy could emerge as a vital component in the multifaceted approach to Alzheimer’s treatment, alongside traditional methods.
Exploring Immune Therapies in Alzheimer’s Treatment
The integration of immune therapies into Alzheimer’s treatment represents a paradigm shift from conventional methods, traditionally focused on symptomatic relief. Immune therapy for Alzheimer’s, particularly involving checkpoint molecules like TIM-3, presents an opportunity to modify the underlying pathology of the disease. By harnessing immune modulation, researchers hope to develop treatments that not only slow cognitive decline but also revitalize the brain’s immune response against damaging plaques.
The rise of interest in immune therapies coincides with a growing understanding of the immune system’s role in neurodegenerative diseases. Early trials of immunotherapeutic approaches have yielded mixed results, but recent advancements in targeting specific pathways—such as those regulated by TIM-3—provide a more focused strategy. By shifting the paradigm towards immune intervention, we pave the way for innovative therapies that aim to restore cognitive function to Alzheimer’s patients and improve quality of life.
The Impact of Microglial Activity on Alzheimer’s Progression
Microglial cells play a crucial role in the progression of Alzheimer’s disease. These immune cells are responsible for maintaining homeostasis in the brain, but when their activity is compromised—as seen with the overexpression of TIM-3—they become less capable of clearing amyloid plaques. The inability of microglia to perform their function leads to the detrimental effects of plaque accumulation, contributing to neurodegeneration and cognitive deficits. A proper understanding of microglial activity could illuminate potential therapeutic pathways.
Recent research has indicated that enhancing microglial function could dramatically influence the course of Alzheimer’s disease. By targeting TIM-3 and other checkpoint molecules, therapies could be developed to restore microglial effectiveness, facilitating the removal of amyloid plaques. This approach illustrates the significance of immune cells in combating Alzheimer’s and their potential role as targets for innovative treatments that address the root cause of the disease rather than just alleviating its symptoms.
Checkpoint Molecules: Bridging Cancer and Alzheimer’s Therapies
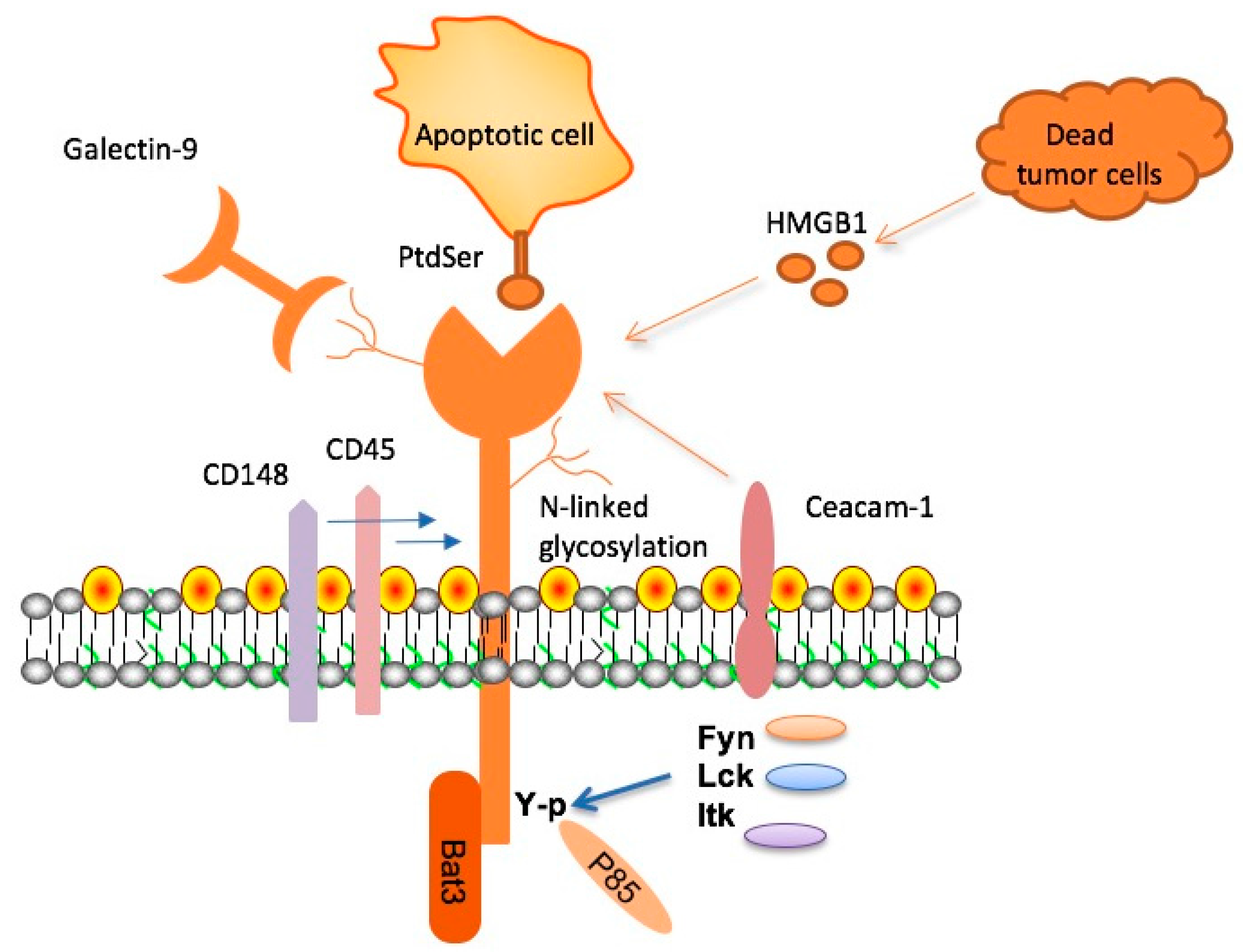
The crossover between cancer treatment strategies and Alzheimer’s therapies is increasingly becoming a focal point in neurological research. Checkpoint molecules, previously explored in oncology for their role in inhibiting T cell function against tumors, are now being examined for their potential in immunology related to Alzheimer’s treatment. The dual nature of TIM-3, acting as both an immune regulator and an inhibitory factor in Alzheimer’s pathology, highlights the potential for repurposing existing treatments in novel ways.
Recognizing that similar immune checkpoints influence both cancer and neurodegenerative diseases provides a unique opportunity for the development of multifaceted therapeutic strategies. The application of immune therapies that have shown efficacy in cancer—such as those targeting TIM-3—can potentially translate into significant advancements for Alzheimer’s treatments. This innovative approach not only informs our understanding of disease mechanisms but also promotes cross-disciplinary collaboration in the research of immunological pathways.
Emerging Research in Alzheimer’s Immunotherapy
The exploration of immunotherapy, particularly involving checkpoint molecules such as TIM-3, is at the forefront of Alzheimer’s research. As scientists delve deeper into how these immune regulators operate, there is a growing excitement about the potential they hold for treating Alzheimer’s disease. By strategically targeting molecules that inhibit microglial activity, researchers aim to enhance the brain’s innate ability to clear amyloid plaques and restore cognitive function. This emerging field of research could revolutionize Alzheimer’s treatment by offering new avenues for intervention.
Recent findings have underscored the importance of TIM-3 in modulating microglial responses to Alzheimer’s pathology. Studies show that inhibiting this checkpoint molecule can lead to significant improvements in plaque clearance and cognitive behavior in mouse models. This opens the door for the development of specific TIM-3 therapies that could harness the immune system’s power to tackle the challenges posed by Alzheimer’s. As research continues to advance, the prospect of effective immunotherapy for Alzheimer’s appears more attainable.
The Future of Alzheimer’s Therapies: A Multi-Targeted Approach
The future landscape of Alzheimer’s therapies is likely to be characterized by a multi-targeted approach, integrating various treatment modalities. While the focus on amyloid plaques has been prominent, there is increasing recognition that factors such as neuroinflammation, immune modulation, and the role of microglia are equally significant. By exploring strategies that involve checkpoint molecules like TIM-3, the field can advance beyond one-dimensional treatments toward more comprehensive therapeutic solutions.
Combining approaches that address multiple aspects of Alzheimer’s pathology—such as plaque accumulation, neuroinflammation, and synaptic dysfunction—presents an opportunity for enhanced patient outcomes. As research on TIM-3 and its effects on microglial function progresses, we can expect the development of therapies that not only mitigate the symptoms but also target the underlying mechanisms of Alzheimer’s disease. This comprehensive outlook will provide hope for patients and their families, as well as a pathway towards more effective Alzheimer’s treatments.
The Importance of Collaboration in Alzheimer’s Research
As the complexity of Alzheimer’s disease unfolds, the importance of collaboration in research becomes increasingly clear. The investigation of TIM-3 as a target for immunotherapy, for instance, has involved multidisciplinary teams bringing together insights from neurology, immunology, and molecular biology. Such collaborative efforts are essential in tackling the multifaceted nature of Alzheimer’s and opening new pathways for effective treatment strategies.
Collaborative research not only enhances the breadth of knowledge but also fosters innovation in therapeutic approaches. By combining expertise from diverse fields, researchers can better understand how immune responses interact with neurodegenerative processes. This will be critical in developing the next generation of treatments that utilize immune modulation, potentially transforming how Alzheimer’s disease is treated. The future of Alzheimer’s research—and the hope it brings for those affected—depends heavily on the synergy of collaborative scientific efforts.
Frequently Asked Questions
What is TIM-3 therapy for Alzheimer’s and how does it work?
TIM-3 therapy for Alzheimer’s targets the inhibitory molecule TIM-3, which inhibits microglia, the brain’s immune cells, from clearing amyloid plaques associated with Alzheimer’s disease. By using anti-TIM-3 antibodies or small molecules to block TIM-3, the immune response is enhanced, allowing microglia to effectively attack and remove these harmful plaques, potentially improving cognitive function.
How does TIM-3 therapy relate to immune therapy for Alzheimer’s?
TIM-3 therapy is a form of immune therapy for Alzheimer’s that utilizes the understanding of immune checkpoints, similar to approaches used in cancer treatments. By inhibiting TIM-3’s function, this therapy aims to restore the microglia’s ability to attack amyloid beta plaques in the brain, addressing a critical aspect of Alzheimer’s pathology.
What are the potential benefits of TIM-3 therapy for Alzheimer’s patients?
The potential benefits of TIM-3 therapy for Alzheimer’s patients include improved clearance of amyloid plaques by activated microglia and enhanced cognitive function. Research has shown that blocking TIM-3 in animal models leads to better memory performance and reduced plaque burden, suggesting that this approach could lead to meaningful advancements in Alzheimer’s treatment.
Why is TIM-3 significant in late-onset Alzheimer’s disease?
TIM-3 is significant in late-onset Alzheimer’s disease because it has been identified as a genetic risk factor linked to the disease. Higher expression levels of TIM-3 in microglia of Alzheimer’s patients can inhibit the immune response needed to clear amyloid plaques, contributing to the progression of the disease. Targeting TIM-3 may help restore the normal function of microglia.
How do microglia and TIM-3 interact in Alzheimer’s disease?
In Alzheimer’s disease, microglia, the brain’s immune cells, express high levels of TIM-3, which suppresses their activity and prevents them from clearing amyloid plaques. This interaction creates an environment where plaque accumulation is unchecked, leading to cognitive decline. TIM-3 therapy seeks to disrupt this inhibitory pathway, reactivating microglia to effectively battle plaque buildup.
Could TIM-3 therapy be combined with existing Alzheimer’s treatments?
Yes, TIM-3 therapy could potentially be combined with existing Alzheimer’s treatments, particularly those targeting amyloid plaques. Since TIM-3 selectively acts on the brain’s immune response, integrating this therapy with other anti-amyloid therapies may enhance overall treatment efficacy and lead to improved patient outcomes.
What new insights about Alzheimer’s treatment does TIM-3 therapy provide?
TIM-3 therapy provides new insights into Alzheimer’s treatment by highlighting the role of the immune system in fighting dementia. It shows that boosting the immune response via checkpoint molecules like TIM-3 can offer a novel approach to treating Alzheimer’s, moving away from traditional focus solely on amyloid-targeting strategies.
What challenges exist in developing TIM-3 therapy for Alzheimer’s?
Challenges in developing TIM-3 therapy for Alzheimer’s include ensuring that the treatment can effectively penetrate the blood-brain barrier, managing potential immune side effects, and demonstrating significant cognitive improvements in clinical trials. However, recent research has shown promise in animal models, paving the way for further human studies.
| Key Point | Detail |
|---|---|
| Research Overview | Study shows TIM-3 molecule may help treat Alzheimer’s, drawing from cancer treatment strategies. |
| Role of TIM-3 | TIM-3 is a checkpoint molecule that inhibits microglia from clearing amyloid plaques in Alzheimer’s patients. |
| Mechanism of Action | Deleting TIM-3 allows microglia to attack plaques, potentially improving memory in mice models. |
| Importance of Microglia | Microglia are the brain’s immune cells, crucial for clearing debris and maintaining cognitive function. |
| Therapeutic Approach | Potential treatments may involve anti-TIM-3 antibodies to boost microglial activity against plaques. |
| Research Development | Team conducted experiments over five years to explore TIM-3’s role in plaque clearance. |
| Future Directions | Next steps include testing anti-TIM-3 therapies in mouse models with human genetic components. |
Summary
TIM-3 therapy for Alzheimer’s shows promise as researchers explore new methods to combat this challenging disease. Recent studies indicate that TIM-3, traditionally associated with the immune response in cancer, can be targeted to enhance the brain’s ability to clear amyloid plaques. By inhibiting TIM-3, microglia can be rejuvenated to engage in plaque clearance, leading to improvements in memory functions observed in mouse models. This innovative approach could pave the way for effective therapies in humans, offering hope against Alzheimer’s as research continues to advance.